COVID patients with lingering symptoms finding relief at new clinics
NEW YORK - COVID-19 came early for Catherine Busa, and it never really left.
The 54-year-old New York City school secretary didn’t have any underlying health problems when she caught the coronavirus in March, and she recovered at her Queens home.
But some symptoms lingered: fatigue she never experienced during years of rising at 5 a.m. for work; pain, especially in her hands and wrists; an altered sense of taste and smell that made food unappealing; and a welling depression. After eight months of suffering, she made her way to Jamaica Hospital Medical Center — to a clinic specifically for post-COVID-19 care.
"I felt myself in kind of a hole, and I couldn’t look on the bright side," Busa said. She did not feel helped by visits to other doctors. But it was different at the clinic.
RELATED: Unemployment claims fall to a still-high 900,000
"They validated the way I felt," she said. "That has helped me push through everything I’m fighting."
The clinic is one of dozens of such facilities that have cropped up around the U.S. to address a puzzling aspect of COVID-19 — the effects that can stubbornly afflict some people weeks or months after the infection itself has subsided.
The programs' approaches vary, but they share the goal of trying to comprehend, treat and give credence to patients who cannot get free of the virus that has infected more than 24 million Americans and killed about 400,000.
"We know this is real," said Dr. Alan Roth, who oversees the Jamaica Hospital clinic. He has been grappling with body pain, fatigue and "brain fog" characterized by occasional forgetfulness since his own relatively mild bout with COVID-19 in March.
Like so much else in the pandemic, the scientific picture of so-called long-haulers is still developing. It’s not clear how prevalent long-term COVID problems are or why some patients keep suffering while others do not.
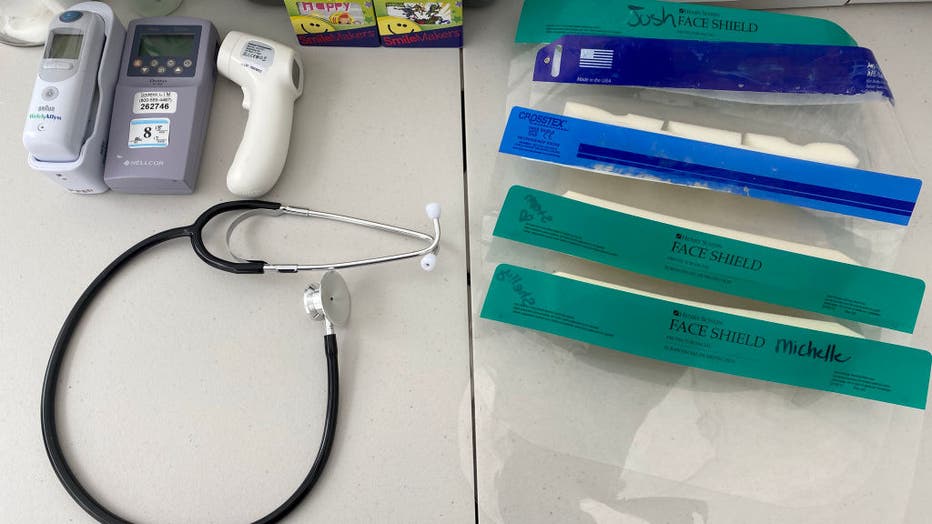
WEST COVINA, CA - APRIL 07: Face masks, digital thermometers and Stethoscope during Coronavirus testing by the city of West Covina and AltaMed in West Covina on Tuesday, April 07, 2020. (Photo by Keith Birmingham/MediaNews Group/Pasadena Star-News vi
Current indications are that up to 30% of patients continue to have significant problems that intrude on daily life two to three weeks after testing positive. Perhaps as many as 10% are still afflicted three to six months later, according to Dr. Wesley Self, a Vanderbilt University emergency physician and researcher who co-wrote a July report from the Centers for Disease Control and Prevention.
Doctors have known for months that intensive care patients can face extended recoveries. But many COVID-19 long-haulers were never critically ill.

Catherine Busa rides an exercise bike as part of her recovery from COVID-19 at her home in New York, Wednesday, Jan. 13, 2021. (AP Photo/Seth Wenig)
At the University of Texas Medical Branch’s post-COVID-19 clinic in Clear Lake, patients range in age from 23 to 90. Half were never hospitalized, said the clinic's director, Dr. Justin Seashore.
"They were told they should be feeling better, and they didn’t," he said. Instead, they were left with fatigue, shortness of breath, anxiety, depression, difficulty concentrating or other problems they did not have before.
Get breaking news alerts in the FOX5NY News app. Download for FREE!
Some were told they would have to be on oxygen for the rest of their lives. A highlight has been helping many of them get off it through treatment that can include respiratory therapy, occupational therapy, mental health check-ins and more, Seashore said.
Long-term COVID-19 care has been launched in settings ranging from big research hospitals like New York’s Mount Sinai, which has over 1,600 patients, to St. John’s Well Child and Family Center, a network of community clinics in south Los Angeles.
RELATED: Appointments canceled for 23,000 New Yorkers due to lack of vaccine, says de Blasio
Rather than focusing specifically on patients who still feel sick, St. John’s aims to schedule a physical exam, a behavioral health visit and monthly follow-ups with everyone who tests positive at one of its clinics, CEO Jim Mangia said. Nearly 1,000 patients have come in for exams.
Since Luciana Flores contracted the virus in June, she has been contending with back pain, stomach problems, shortness of breath and worry. The mother of three lost her job at a laundry amid the pandemic, and she doesn't feel well enough to look for work.
St. John's has helped, she said, by diagnosing and treating a bacterial infection in her digestive system.
"I think it's really important for other patients to receive the same care," Flores, 38, said through a Spanish interpreter. "I don’t feel the same. I don’t think anything will ever be the same, but there’s no other way around it: I have to keep moving forward."
There’s no proven cure for long-term COVID problems. But clinics aim to offer relief, not least by giving patients somewhere to turn if their usual doctor can't help.
"We wanted to create a place that patients could get answers or feel heard," even if there are still unanswered questions, said Dr. Denyse Lutchmansingh, the clinical lead physician at Yale Medicine’s Post-COVID Recovery Program.
At the Jamaica Hospital program, patients get mental health assessments, a lung specialist's attention and physical exams that delve deeper than most into their lifestyles, personal circumstances and sources of stress. Several hundred people have been treated so far, Roth said.
The idea is to help patients "build their own healing capacity," said Dr. Wayne Jonas, former director of the National Institutes of Health’s Office of Alternative Medicine. He is now with the Samueli Foundation, a California-based nonprofit that works with the hospital on marrying alternative ideas with conventional medicine.
The long-haulers get exercise and diet plans and group or individual mental health sessions. Recommendations for supplements, breathing exercises and meditation are also likely. That's in addition to any prescriptions, referrals or primary care follow-ups that are deemed necessary.
RELATED: CDC forecast now projects up to 508,000 COVID-19 deaths by Feb. 13
"We're not just saying, ‘It’s all in your head, and we're going to throw herbs and spices at you,'" Roth said. With no tidy, proven answer for the complex of symptoms, "we do a common-sense approach and take the best of what's out there to treat these people."
Busa got a test that determined she has sleep apnea, which causes people to stop breathing while asleep and often feel fatigued when awake. She is getting a device for that and is using wrist braces and getting injections to ease her pain. Her program also includes psychotherapy appointments, supplements and new daily routines of walking, riding a stationary bike and writing in a journal about what she has to feel grateful for.
Busa feels she is coming along, especially in terms of her mood, and credits the clinic.
"There's light at the end of the tunnel," she said, "and there are people and doctors out there who can relate to you."

